The UK’s first mobile burns unit has treated more than 700 patients in its first six months, helping to close gaps in access to healthcare across the East of England. Nurses from the St Andrew’s Burns Unit, based at Broomfield Hospital in Chelmsford, say the Burns Outreach Bus has already reduced health inequalities by providing at-home care to people who might otherwise struggle to attend appointments.
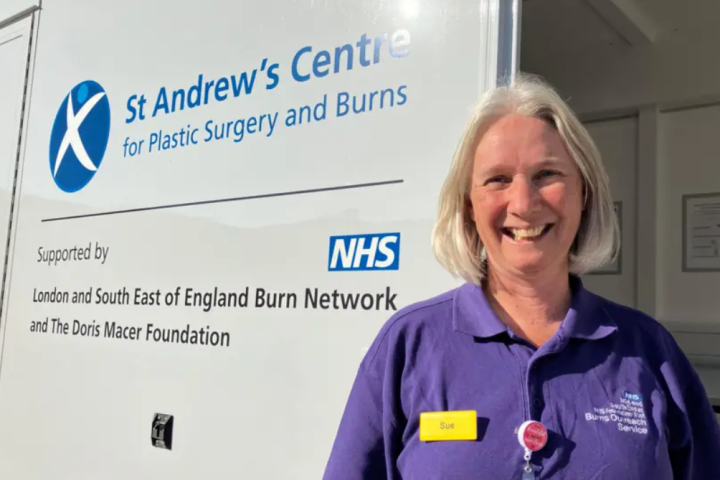
In total, the bus is estimated to have saved patients around 29,300 miles in travel — equivalent to about 128 flights from London to Paris. Advanced nurse practitioner Sue Boasman, who leads the project, said the service had reached communities across Suffolk, Norfolk, Cambridgeshire, Peterborough, Hertfordshire, Kent, and even parts of London.
“The reality is some patients are choosing between feeding their families a hot meal and coming to a burns appointment,” she said. “That’s what they’re feeding back to us.” The Burns Outreach Bus allows nurses to visit people in their homes to change dressings, monitor wounds, and provide recovery advice. Typically, it serves around eight to ten patients per day.
The bus was launched earlier this year as part of a one-year pilot funded by the London and South East Burns Network and the Doris Macer Foundation. It is run by the Mid and South Essex NHS Foundation Trust, which oversees Broomfield Hospital. Chief medical officer Christine Blanshard said the initiative had already made “a real difference” to patients’ lives.
“We are committed to supporting this innovative way of working,” she said. “The service supports people in the wider East of England area and reduces health inequalities by providing burns care for patients who find it hard to travel. We are supporting the team in exploring future options for the service.”
Because burn patients are at high risk of infection, maintaining a sterile and comfortable environment inside the bus was one of the team’s top priorities. “This is the UK’s first burns bus, so we kind of made it up as we went along,” Ms Boasman said. “It’s important that it’s kept clean and that it’s easily cleanable, but we also want patients to feel safe and welcome when they come in for wound care.”
On Tuesday, members of the public were invited to Southend University Hospital to learn more about the bus and its work. Visitors met “Toothless Ted,” a training dummy used to demonstrate burn treatment techniques, and heard from the nurses leading the outreach project. Ms Boasman hopes the bus will continue beyond its initial pilot year, especially after seeing how it has improved access to care for vulnerable groups.
Burns are among the most common forms of trauma worldwide, ranking fourth after road accidents, falls, and violence. The World Health Organization estimates that around 180,000 people die every year from burn-related injuries, most in low- and middle-income countries. In the UK, approximately 250,000 people sustain burn injuries each year. Around 175,000 of them attend emergency departments, and 16,000 require specialist hospital care. The majority — about 90% — are classified as non-complex burns that can be treated outside of hospital settings.
Children are particularly vulnerable: they account for nearly half of all severe burn cases, and those under five make up between 50% and 80% of childhood burns. Burns are the eleventh most common cause of death in children aged one to nine, and the fifth most common cause of non-fatal injury. Certain groups face higher risks — including elderly people, those with mobility issues, or those with cognitive or sensory impairments that make it harder to react quickly to danger.
Complications from burns can range from infection and hypothermia to toxic shock syndrome and long-term scarring. Recovery often requires multiple dressing changes, physiotherapy, and psychological support — services that can be difficult to access for people living far from specialist hospitals. That’s where the Burns Outreach Bus comes in. By bringing treatment directly to patients’ homes, the mobile unit reduces travel costs, improves continuity of care, and lowers the risk of infection for people who are housebound or financially struggling.
It also helps reduce pressure on hospitals, freeing up resources for the most severe or complex burn cases. The NHS team behind the project believes the model could be replicated elsewhere in the UK, not only for burn care but for other types of specialist community healthcare. For now, Ms Boasman and her colleagues are focused on keeping the bus on the road. “We’ve seen firsthand how much this service means to people,” she said. “It’s helping them heal — not just physically, but emotionally, too.”